Peripheral Vascular Disease (PVD)
Description
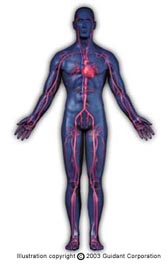
- Peripheral vascular disease, or peripheral artery disease, are caused by the same atherosclerotic plaque that causes coronary artery disease. Frequently atherosclerosis is not confined to one artery but may involve arteries in other areas as well. Some of the more commonly affected peripheral areas are the arteries in the legs, arms, kidneys and neck. Some patients may have both coronary artery disease and peripheral vascular disease.
- As the internal lining of the artery thickens from the atherosclerotic plaque, the blood vessel becomes increasingly constricted and blood flow diminishes. Therefore, the symptoms you may experience depend on what artery is affected and how severely the blood flow is reduced.
 Some of the symptoms you may experience in the affected areas are:
Some of the symptoms you may experience in the affected areas are:- Claudication (dull, cramping pain in hips, thighs or calf muscle)
- Buttock pain
- Numbness or tingling in leg, foot or toes
- Changes in skin color (pale, bluish or reddish discoloration)
- Changes in skin temperature, coolness
- Impotence
- Infection/sores that do not heal
- Ulceration or gangrene
- Uncontrolled hypertension (high blood pressure)
- Renal failure
Risk Factors
- Clinical studies have identified factors that increase the risk of peripheral vascular disease. Some of these factors cannot be changed while others can be managed to greatly reduce your risk of the disease.
- Diabetes: Peripheral vascular disease is not uncommon among those individuals with diabetes. This correlation is due to complications of the disease which may cause damage to the large and small blood vessels of the legs and feet.
- Smoking: The risk of peripheral vascular disease is dramatically increased in smokers. When a person stops smoking, regardless of how much he or she may have smoked in the past, their risk of peripheral vascular disease rapidly declines.
- Any of the following risk factors may also increase your chance of developing peripheral vascular disease:
- Obesity (being overweight)
- High blood pressure
- A family history of the disease
- Lack of exercise
- Coronary artery disease
- Over the age of 65
- Hyperlipidemia (high cholesterol)
Diagnosis
- If your doctor suspects that you have peripheral vascular disease or if you have symptoms of the disease, several tests are used to make a diagnosis. Diagnostic tests that your doctor may order include Ankle Brachial Index (ABI), Ultrasound Doppler Test, and Angiogram.
Treatment
Many treatments can be used to improve blood flow through the peripheral arteries. The latest interventions for treating peripheral vascular disease can bring relief and are more cost effective than surgery. Most procedures require no more than an overnight hospital stay, and patients enjoy an early return to most normal activities. Techniques available to you include:
- Angioplasty and Stents
- Atherectomy - a minimally invasive intervention procedure that involves the excision and removal of blockages by catheters with miniature cutting systems.
All of these techniques treat the build-up of plaque by either removing it, compressing it or displacing it. During these procedures the physician will periodically inject a contrast dye and take x-ray pictures to determine whether or not the artery is sufficiently opened. If the blockage is extremely long or has become very hard and calcified with time, it may be resistant to any of these interventions. In these cases, surgery may be required to bypass the problem area.
Non-invasive interventions may also be used to treat Peripheral Vascular Disease. These interventions include:
- Exercise - exercise may improve arterial blood flow to the affected limb. Exercise is not recommended for people with severe rest pain, venous ulcers, or gangrene. Consult your doctor before beginning an exercise program.
- Positioning - It is recommended that people do not cross their legs, which may interfere with blood flow. Some people manage swelling by elevating their feet at rest. You should elevate your feet but not above the heart level. Extreme elevation slows arterial blood flow to the feet. Again, talk with your doctor about positioning.
- Promoting Vasodilation (increasing the diameter of blood vessels) - Vasodilation can be achieved by providing warmth to the affected extremity and preventing long periods of exposure to cold. It is recommended that people maintain a warm environment at home and wear socks or insulated shoes at all times. Never apply direct heat to the limb, such as with the use of a heating pad ore extremely hot water to reduce the risk of burns.
- Stop Smoking - Smoking causes vasoconstriction (decreases the diameter of blood vessels), which can interfere with adequate blood flow to the limbs. Emotional stress, exposure to cold temperatures, and caffeine can all cause vasoconstriction.
- Medications - Prescribed medications are often given to patients with chronic peripheral vascular disease. Antiplatlet medications (such as Aspirin and Plavix) may be prescribed. Other medications may be prescribed depending on the patient's condition.
- Controlling Hypertension - Controlling high blood pressure can improve blood flow through the blood vessels and reduce the constriction of blood vessels.
- Aneurysm
- Aortic Dissection
- Atrial Fibrillation
- Blood Clot (Thrombosis)
- Chest Pain or Discomfort (Angina)
- Coronary Artery Disease
- Diabetes
- Heart Attack (Acute Myocardial Infarction)
- Heart Failure
- Heart Rhythm Disorders
- High Blood Pressure (Hypertension)
- Peripheral Vascular Disease (PVD)
- Stroke
- Sudden Cardiac Death
